Mind and behavior
Psychology may be the scientific study of the mind and behavior, but not to the exclusion of the physical seat of the mind, the brain. The interplay between physical and non-physical is as central to research and treatment as it is to everyday life. Within the seemingly isolated topics of depression, anxiety, and memory loss, for example, an important question is taking on attention: Can Depression And Anxiety Cause Memory Loss?
The human brain is a frontier under constant exploration. It’s not unlike the infinite universe that boggles the non-astronomical mind. For every discovery made, a new galaxy opens. More questions. More theories. And more research.
Take depression, for example. While contemporary psychology may employ a wide array of therapies to treat it, depression has a startling history of far-reaching diagnoses and “treatments.”
In the second millenium B.C.E., “experts” treated depression, like most illnesses, as a spiritual condition – the result of demonic possession.
Through the ages, theories have evolved. And “treatments” have run an often frightening course – from witch hunts to bloodletting to frontal lobotomies.

Today we tread with compassion and the backing of science in the quest for truth and treatment. Depression, like anxiety and other forms of mental illness, now has a voice and a spotlight for deeper understanding. Thank goodness.
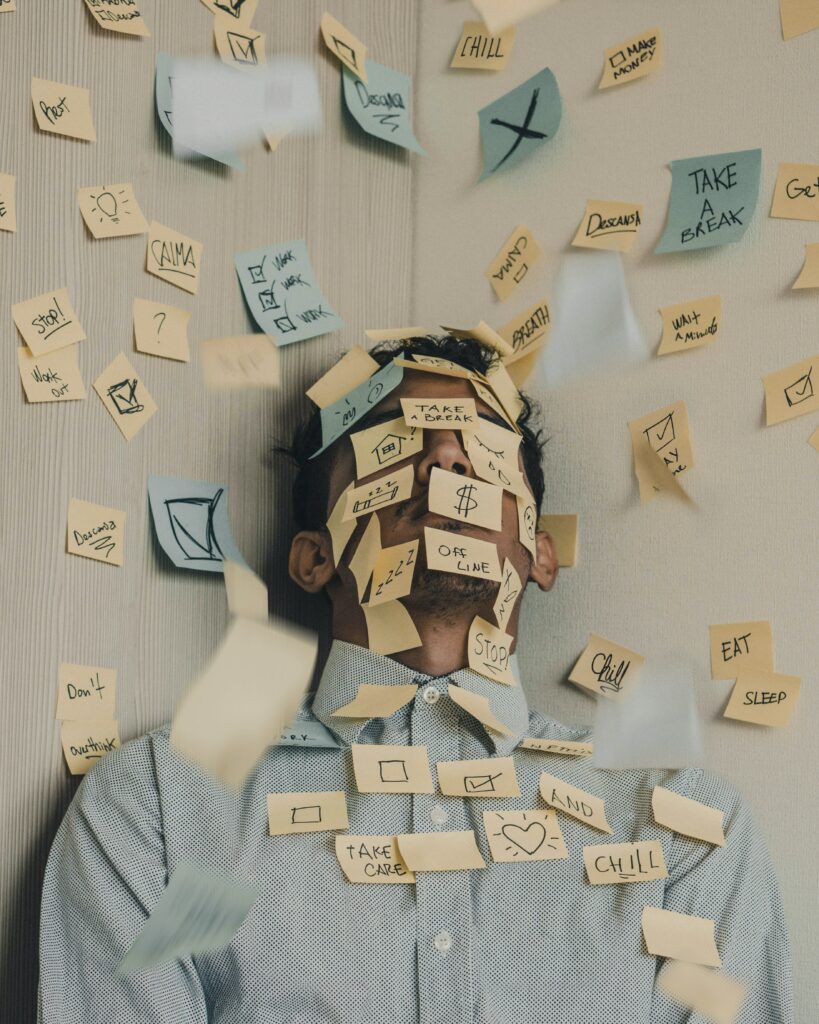
One of the common complaints of those who suffer from depression and/or anxiety is memory loss, or cognitive impairment.
Specifically, the working/short-term memory is affected. Words, names, directions, executive functioning, decision-making, locating and misplacing objects – the crazy-making stuff that adds insult to injury.
The long-term memory – remembering key events and people from your life, for example – remains intact.
What’s the connection here? How is it that suffering from low mood, disinterest, irritability, hopelessness, and other symptoms of depression can wreak havoc with basic mental tasks?
With regard to depression, we know for certain it’s linked to structural and chemical changes in the brain. And these changes can begin at the onset of depression and even continue after depressive symptoms have been resolved.
Specifically, the affected areas are the prefrontal cortex, hippocampus, and amygdala. These areas are all involved in cognition and emotional processing, connected neurally via synapses and neurotransmitters. What affects one affects all.
In addition to the interconnection of these areas, there’s also overlap with the stress response systems.
In other words, your mood, cognition, and ability to handle stress are all firing off the same circuitry.
The way depression and anxiety cause memory loss has to do with stress.

The body’s stress response system is masterfully designed to engage during fight-or-flight situations. It triggers a cascade of changes that can be life-saving if you’re engaged in a staredown with a predator.
But it can also be counterproductive if it overstays its welcome or gets triggered in situations that don’t warrant it. (In that regard, one might wonder if perhaps the stress response hasn’t caught up with human evolution.)
Those who suffer from chronic anxiety, with or without depression, know the constant worry and fear, also known as are trademarks of the condition.

Everything is a perceived threat. A headache, a flat tire, something a loved one says (or doesn’t say), a message from Human Resources – it all triggers a stress response. And in flows the cortisol that, under acutely threatening situations, would sharpen the mind and give the body superhero powers.
But day in and day out? That kind of chronic stress response does more harm than good.
Add in the lack of sleep that usually accompanies anxiety, and “brainpower” spreads itself thin – or diminishes altogether.
What many people inexperienced with clinical depression don’t understand is the difference between situational sadness and chronic depression.
Everyone experiences periods of sadness, irritability, anxiety, and grief. But people who live with clinical depression don’t bounce back as quickly.
And the longer one lives with depression, the more permanent the effects become.
From a purely physical standpoint, depression related memory loss can be attributed to depression’s three startling effects on the brain:
- shrinkage (of the hippocampus, prefrontal cortex, and thalamus)
- inflammation
- decreased oxygen supply
When you think about the physical effects of anxiety and depression, chances are they’re effects you can actually sense. You feel your hands sweating, your heart racing, your head hurting. And you see the change in your weight from the change in your eating habits.
You also feel the frustration of not being able to complete everyday tasks. You’re distracted, preoccupied, exhausted, disinterested.
But your brain shrinking? Being inflamed? Not getting enough oxygen?
This all starts to sound like the defining brain atrophy of Alzheimer’s.
And that raises even more questions and cause for research.
If depression and anxiety cause memory loss, how do we need to change the narrative around these disorders?
And around mental health in general?
How do science, medicine, psychiatry, and psychology improve on the detection, intervention, treatment, and management of depression and anxiety?
If depression and anxiety can cause memory loss, is the reverse equally true or at least plausible? Can memory loss cause depression and anxiety in an otherwise non-depressed person?
Can we medically stop or reverse the changes to the brain caused by depression and anxiety?
If medical and psychological intervention can keep sufferers flourishing despite anxiety and depression, can memory loss be mitigated?
If depression, anxiety, and memory loss can co-occur symptomatically, can a “cure” for one hold the key to curing the others?
In the frontier of the human brain and mind, there will always be more questions than answers.
But look how far we’ve come.
Dr Elayne Daniels is a MA based psychologist, international and coach, specializing in eating disorder recovery, anxiety and depression, and body image. She especially enjoys working with Highly Sensitive People.


